A Herbal Perspective on Delayed Gastric Emptying
When one of the foundational figures in Ayurveda, stated ‘Shashkuli Amla Pitta Karanam’ he was indeed making a direct connection between a specific fried snack, Shashkuli, and the development of Amla Pitta. While Amla Pitta isn't an exact one-to-one translation of modern GERD, its symptoms like sour belching, heartburn, and indigestion are strikingly similar to the reflux-like discomfort many experience today. This wasn't just an observation; it was a clear declaration that dietary choices directly impact gastrointestinal well-being, leading to specific health problems.
Similarly, in Traditional Chinese Medicine, Li Dongyuan, through his seminal work "Pi Wei Lun" (Treatise on the Spleen and Stomach), stressed the paramount importance of stomach health. When he spoke of "internal damage as a primary cause of all abnormalities, he was unequivocally pointing to the gut. For Li Dongyuan, the Spleen and Stomach were the source of all post-natal energy, and their dysfunction, often due to improper diet, overwork, or emotional stress, could cascade into systemic illness. His insights into conditions manifesting as epigastric pain, bloating, indigestion, and altered appetite directly align with what we now categorize as various forms of gastritis and functional dyspepsia.
Modern biomedicine grapples with a variety of gut disorders, many of which present with overlapping symptoms and can be challenging to diagnose. Consider conditions like GERD (Gastroesophageal Reflux Disease), delayed gastric emptying, and functional dyspepsia; they often share similar symptoms and may even stem from related underlying causes (Egboh et al., 2025). Even when an endoscopy reveals no erosion or damage to the mucosal lining, a patient might still experience symptoms consistent with dyspepsia and GERD (Kamiya et al., 2009).
This article focuses on Delayed Gastric Emptying. It will explore this condition and discuss animal studies examining the effects of Chinese and Ayurvedic herbs on Delayed Gastric Emptying and Dyspepsia.
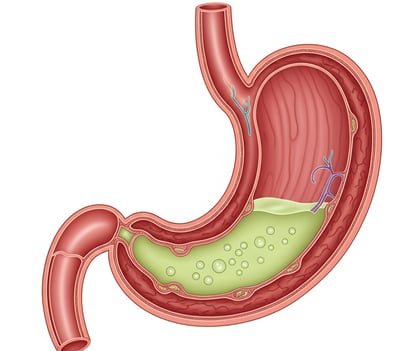
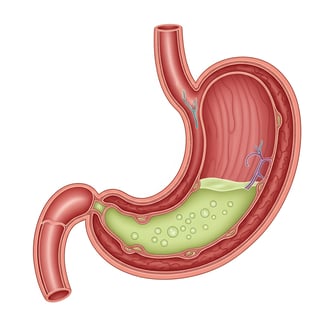
What is Delayed Gastric Emptying or Gastroparesis?
Gastroparesis, according to Wang and Camilleri (2022), is a motility disorder characterized by delayed gastric emptying in the absence of mechanical blockage. The authors also note the symptomatic similarities between GERD and Gastroparesis. However, a key distinguishing symptom of gastroparesis is the postprandial vomiting of undigested food.
Clinically patients might come with a history of abdominal surgery(Shafi & Pasricha, 2007) or Diabetes(Aswath et al., 2023) with symptoms include nausea, vomiting, early satiety, postprandial fullness, and, in some patients, upper abdominal pain. Most patients have nausea and early satiety. In 146 patients with gastroparesis, nausea was present in 92%, vomiting in 84%, abdominal bloating in 75%, early satiety in 60%, and abdominal pain in 46%.(Wang and Camilleri 2022)
Diagnosis
Gastroparesis diagnosis involves confirming delayed stomach emptying in a patient experiencing symptoms, after ruling out any physical blockage through an endoscopy. If no obstruction is found, a gastric emptying test is performed. A common method is scintigraphy, which uses a radiolabeled solid meal and monitors gastric emptying over a four-hour period.(Wang and Camilleri 2022)
Chinese Medicine Approach
Traditional Chinese medicine views Delayed Gastric Emptying as stemming from the interplay between the Spleen and Liver organs. Patient diagnoses will vary, presenting as either Spleen deficiency or Liver overacting on the Spleen. However, a fundamental underlying factor is often Spleen Qi deficiency, even with individual patient variations.symptoms like Nausea, Bloating, Tiredness have always come under SPleen organ umbrella.
Symptoms such as nausea, bloating, and tiredness have traditionally been associated with the Spleen organ.
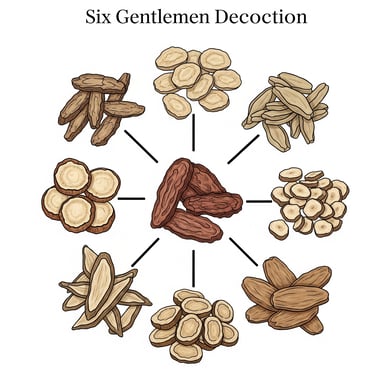
Researches On Chinese Herbs Pertaining to Delayed Gastric Emptying
A study by Tominaga et al. (2011) investigated six gentlemen decoction and its effects on delayed gastric emptying in rats. They found that it significantly suppressed the delay induced by 5-hydroxytryptamine (5-HT) or a 5-HT3 receptor agonist, similar to the known 5-HT3 antagonist ondansetron. Hesperidin, a key ingredient in this formula, showed similar effects. However, it did not reverse dopamine-induced delays. The improvement by six gentlemen Decoction and ondansetron was blocked by atropine, suggesting a role for the cholinergic pathway. The study concluded that this particular formula likely improves delayed gastric emptying through antagonistic action on the 5-HT3 receptor pathway in rats, providing animal model evidence for its prokinetic effects.
Kimura and Sumiyoshi (2012) investigated the traditional herb Atractylodes lancea and its compound β-eudesmol in mice. Their research showed that both the extract and β-eudesmol improved gastric emptying and small intestinal motility. Specifically, they counteracted delays induced by both dopamine and 5-hydroxytryptamine (5-HT), particularly acting as a 5-HT3 receptor antagonist. These animal findings suggest Atractylodes lancea stimulates gut motility by inhibiting dopamine D2 and 5-HT3 receptors, supporting its traditional use for dyspepsia and gastroparesis.
Zhang et al. (2008) demonstrated that Atractylodes lancea essential oil accelerated delayed gastric emptying in stress-induced rats. This effect was mediated by inhibiting central corticotropin-releasing factor (CRF) and activating the vagal pathway, which in turn regulated gastrointestinal hormones. This animal study highlights the herb's potential to address stress-related gastric motility issues.
Nakai et al. (2003) demonstrated that an Atractylodes lancea extract significantly improved delayed gastric emptying in rats induced by nitric oxide inhibition. This prokinetic effect was attributed specifically to four polyacetylenic compounds within the extract, with atractylodin being a key active component. This study provides direct animal evidence for Atractylodes lancea's role in enhancing gastric motility.
Gong et al. (2023) investigated Citrus aurantium and Citrus reticulata extract alone or with Bupleurum chinense on stress-induced delayed gastric emptying in mice. Both combinations significantly reduced gastric residual rates. They increased serotonin (5-HT), motilin (MTL), and substance P (SP) levels, and upregulated 5-HT4R and c-kit expression. The triple combination showed superior prokinetic effects, suggesting combined antidepressant-prokinetic herbal therapies hold promise for gut dysmotility.


Ayurveda Approach
Ayurveda's core principle centers on Agni, the digestive fire responsible for metabolizing food. Delayed Gastric Emptying or Functional Dyspepsia can be linked to a diminished Agni in the stomach, resulting in symptoms like bloating, nausea, and epigastric pain. Therefore, the primary strategy involves enhancing this metabolic fire through appropriate diet and remedies. While treatment is individualized, the fundamental underlying cause invariably relates to Agni, or metabolic fire.
Researches On Ayurveda Herbs Pertaining to Delayed Gastric Emptying
Tamhane et al. (2000) conducted an experimental study in Charles Foster rats to investigate the prokinetic effects of oral Terminalia chebula, an Ayurvedic herb traditionally valued for improving gastrointestinal motility. The study directly compared its efficacy to established conventional prokinetic and antikinetic drugs. Rats receiving oral Terminalia chebula (100 mg/kg/day for 15 days) demonstrated a significantly increased gastric emptying rate (86.57%) compared to the normal control group (51.6%). This prokinetic effect was notably more pronounced than that observed with metoclopramide (76.33%), a common prokinetic medication, and stood in sharp contrast to atropine, which significantly inhibited emptying. These findings provide strong animal evidence supporting the potent prokinetic activity of Terminalia chebula in modulating gastric motility, suggesting its potential as a valuable alternative or complementary agent to modern prokinetic drugs.


Wu et al. (2008) conducted a randomized, double-blind study on 24 healthy volunteers to investigate the effects of ginger (1200 mg) on gastric emptying and antral motility. The study found that ginger significantly accelerated gastric emptying, evidenced by a more rapid decrease in antral area and a significantly shorter gastric half-emptying time (13.1 min with ginger vs. 26.7 min with placebo). Furthermore, ginger ingestion led to a greater frequency of antral contractions. No significant differences were observed in fundus dimensions or postprandial symptoms in these healthy volunteers.These findings provide direct human evidence that ginger can accelerate gastric emptying and stimulate antral contractions, suggesting its potential therapeutic benefit in patient groups experiencing delayed gastric emptying.


As a Synergy
Artichoke and Ginger
A pilot human study by Lazzini, Polinelli, et al. (2016) demonstrated that a standardized extract of ginger and artichoke significantly accelerated gastric emptying in healthy volunteers. Post-meal gastric area was 24% smaller with the extract compared to placebo (p<0.001). This provides direct human evidence supporting the prokinetic effect of this herbal combination.


Conclusion
Both Ayurveda and Traditional Chinese Medicine (TCM) emphasize individualized and systemic approaches over solely treating symptoms. While integrating Western diagnostic techniques is valuable, the foundational principles of these herbal philosophies should remain central. Consider a patient diagnosed with delayed gastric emptying. Simply prescribing herbs without a thorough individual assessment through TCM or Ayurveda is inappropriate. For instance, a person with delayed gastric emptying and excess stomach heat might not benefit from ginger.Furthermore, potential herb-drug interactions are critical to consider, necessitating a careful review of the patient's prescribed medications. While biomedicine recognizes the interconnectedness and overlapping symptoms of conditions like GERD, delayed gastric emptying, and functional dyspepsia, traditional medicine practitioners must adopt a holistic perspective, considering the entire metabolic system.
Most current research on herbal supplements for gastroparesis relies on animal experiments. To gain a clearer understanding of their effectiveness in humans, well-established human studies are essential.
For managing delayed gastric emptying effectively, it's advisable to seek guidance from both a gastroenterologist for medical diagnosis and treatment, and an herbalist to gain a comprehensive, holistic perspective.
References:
Wu, K.-L., Rayner, C. K., Chuah, S.-K., Changchien, C.-S., Lu, S.-N., Chiu, Y.-C., Chiu, K.-W., & Lee, C.-M. (2008). Effects of ginger on gastric emptying and motility in healthy humans. Journal of Gastroenterology and Hepatology, 23(11), 1616–1620.
Tamhane, M. D., Thorat, S. P., Rege, N. N., & Dahanukar, S. A. (1997). Effect of oral administration of Terminalia chebula on gastric emptying: an experimental study. Journal of Postgraduate Medicine, 43(1), 12–13.
Fass, R., McCallum, R. W., & Parkman, H. P. (2009). Treatment challenges in the management of gastroparesis-related GERD. Journal of Clinical Gastroenterology, 5(10 Suppl 18), 4–16.
Aswath, G. S., Foris, L. A., Ashwath, A. K., & Patel, K. (2023, March 27). Diabetic Gastroparesis. StatPearls Publishing.
Kamiya, T., Adachi, H., Hirako, M., & Joh, T. (2009). Impaired gastric motility and its relationship to reflux symptoms in patients with nonerosive gastroesophageal reflux disease. Journal of Gastroenterology, 44(3), 183–189.
Egboh, S.-M., Duncanson, K., Potter, M., Keely, S., & Talley, N. J. (2025, January 22). Functional dyspepsia and gastroparesis: Are they distinct disorders, a spectrum of diseases or one disease?
Tominaga, K., Kido, T., Ochi, M., Sadakane, C., Mase, A., Okazaki, H., Yamagami, H., Tanigawa, T., Watanabe, K., Watanabe, T., Fujiwara, Y., Oshitani, N., & Arakawa, T. (2011). The Traditional Japanese Medicine Rikkunshito Promotes Gastric Emptying via the Antagonistic Action of the 5-HT3 Receptor Pathway in Rats. Evidence-Based Complementary and Alternative Medicine, 2011, 1–11.
Zhang, W.-j., Zhao, Z.-y., Chang, L.-k., Cao, Y., Wang, S., Kang, C.-z., Wang, H.-y., Zhou, L., Huang, L.-q., & Guo, L.-p. (2021). Atractylodis Rhizoma: A review of its traditional uses, phytochemistry, pharmacology, toxicology and quality control. Journal of Ethnopharmacology, 266, 113415.
Kimura, Y., & Sumiyoshi, M. (2012). Effects of an Atractylodes lancea rhizome extract and a volatile component β-eudesmol on gastrointestinal motility in mice. Journal of Ethnopharmacology, 141(1), 345–351
Zhang, H., Han, T., Sun, L.-N., Huang, B.-K., Chen, Y.-F., Zheng, H.-C., & Qin, L.-P. (2008). Regulative effects of essential oil from Atractylodes lancea on delayed gastric emptying in stress-induced rats. Phytomedicine, 15(8), 643–649.
Nakai, Y., Kido, T., Hashimoto, K., Kase, Y., Sakakibara, I., Higuchi, M., & Sasaki, H. (2003). Effect of the rhizomes of Atractylodes lancea and its constituents on the delay of gastric emptying. Journal of Ethnopharmacology, 84(1), 51–55.
Yang, S.-H., Zhu, J., Wu, W.-T., Li, J.-M., Tong, H.-L., Huang, Y., Gong, Q.-F., Gong, F.-P., & Zhong, L.-Y. (2023). Rhizoma Atractylodis Macrocephalae—Assessing the influence of herbal processing methods and improved effects on functional dyspepsia. Frontiers in Pharmacology, 14, 1236656.
Disclaimer: For Educational Purposes Only. This information is not intended as medical advice, diagnosis, or treatment. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.